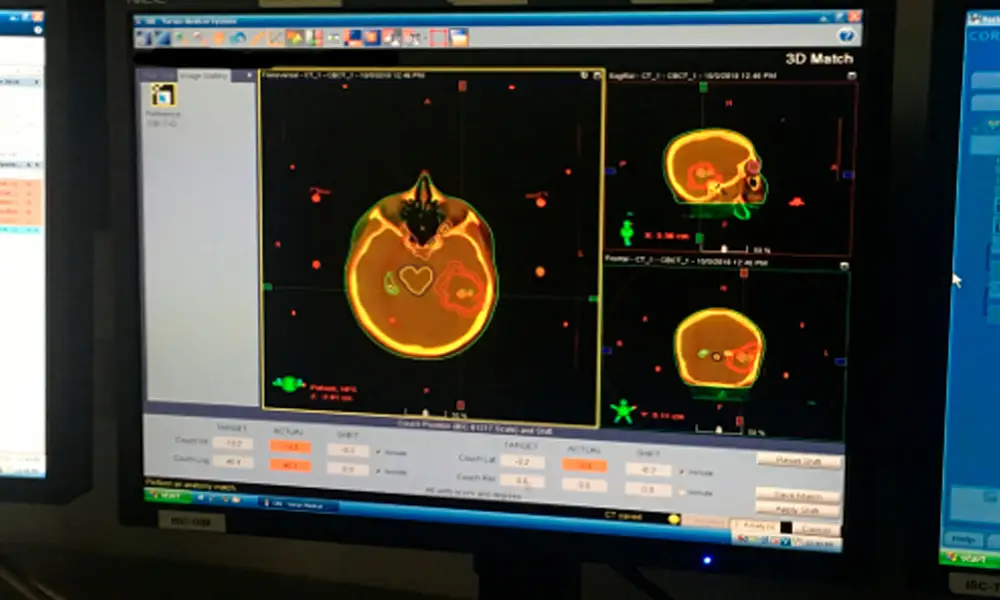
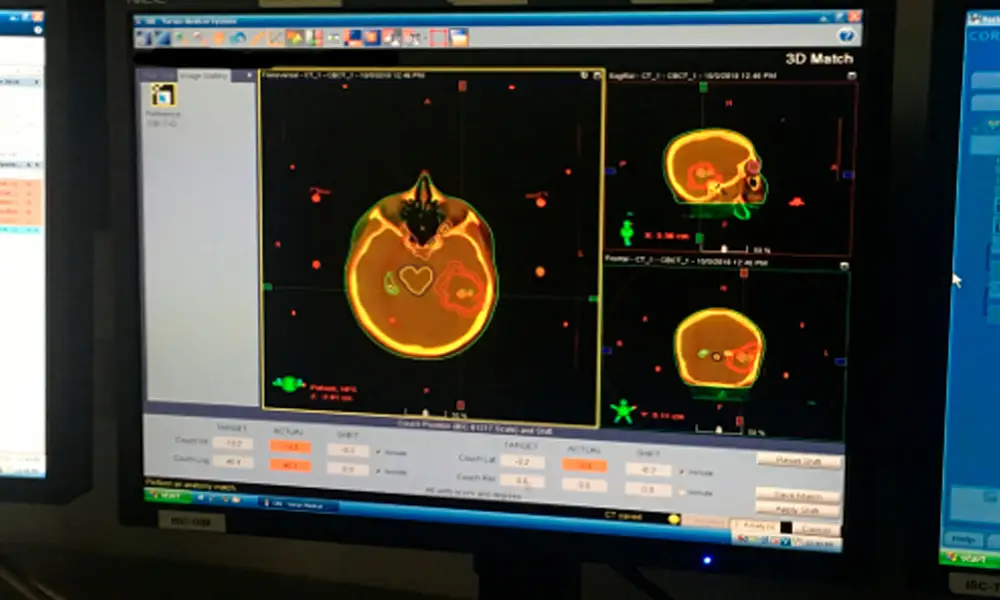
Image-Guided Radiation Therapy (IGRT) combines imaging techniques, such as computed tomography (CT), with radiation therapy during each treatment session. The ability to adjust the position before applying the radiation beam is simply remarkable, as it reduces side effects while targeting the tumor in the exact location each day.
It allows:
The delivery of radiation therapy requires a treatment team, which includes a radiation oncologist, medical physicist, dosimetrist, and imaging technologists. The radiation oncologist is a physician who evaluates the patient and determines the appropriate therapy or combination of therapies and the type of IGRT to be used. The doctor decides which area needs treatment and the dosage to be administered. Together with the medical physicist and dosimetrist, the physician determines which techniques should be used to deliver the prescribed dosage. The physicist and dosimetrist then perform detailed treatment calculations. The imaging technologists are specially trained technologists who acquire images and deliver daily treatments. The radiation oncology nurse assesses the patient and provides additional information about the treatment and potential side effects. The radiation oncology nurse, in collaboration with the physician, also helps manage any reactions or side effects that may occur due to the treatment.
The equipment is operated by an imaging technologist, a highly trained technician. The overall treatment plan is created and monitored by the radiation oncologist, a highly trained physician who specializes in treating cancer with radiation therapy.

Or technologist if there is any possibility that they are pregnant or if they are breastfeeding their baby.
Regarding pregnancy, breastfeeding, and imaging.
Patients with pacemakers or loose metal in their bodies should inform the treatment team if MRI is used for simulation or IGRT.
Reference markers or electromagnetic transponders may be placed inside the body, near or within the tumor, to help the treatment team identify the area.
Or tattooed with colored ink to help align and direct the radiation equipment.
Using ultrasound should drink enough water about an hour before each treatment to keep the bladder full so that the prostate can be imaged or “seen” by the ultrasound machine.
Aside from the routine preparation for radiation therapy, which may include three-dimensional conformal radiation therapy, intensity-modulated radiation therapy, proton beam therapy, or stereotactic body radiation therapy (SBRT).
The Proton Beam Therapy page, or the SBRT page for more information.
Generally, procedures are performed on an outpatient basis. However, it is advisable to prepare for spending half a day or more in the imaging department. You will be informed whether you will need someone to accompany you and take you home after the procedure.
You may be notified not to eat or drink anything after midnight before the treatment. Ask your doctor if you should continue taking your usual medications on the day of treatment and if you should bring your medications with you to the procedure.
How is the procedure performed?
Radiation surgery treatments are similar to taking X-rays. Generally, X-rays cannot be seen, felt, or heard, except for patients receiving treatment in the brain, who may see lights while the machine is on, even with their eyes closed. The treatment itself does not cause any pain or discomfort. If you experience pain for other reasons, such as back pain or discomfort from the head device or immobilization device, please inform the medical or nursing staff.

Image-Guided Radiation Therapy (IGRT) combines imaging techniques, such as computed tomography (CT), with radiation therapy during each treatment session. The ability to adjust the position before applying the radiation beam is simply remarkable, as it reduces side effects while targeting the tumor in the exact location each day.
It allows:
The delivery of radiation therapy requires a treatment team, which includes a radiation oncologist, medical physicist, dosimetrist, and imaging technologists. The radiation oncologist is a physician who evaluates the patient and determines the appropriate therapy or combination of therapies and the type of IGRT to be used. The doctor decides which area needs treatment and the dosage to be administered. Together with the medical physicist and dosimetrist, the physician determines which techniques should be used to deliver the prescribed dosage. The physicist and dosimetrist then perform detailed treatment calculations. The imaging technologists are specially trained technologists who acquire images and deliver daily treatments. The radiation oncology nurse assesses the patient and provides additional information about the treatment and potential side effects. The radiation oncology nurse, in collaboration with the physician, also helps manage any reactions or side effects that may occur due to the treatment.
The equipment is operated by an imaging technologist, a highly trained technician. The overall treatment plan is created and monitored by the radiation oncologist, a highly trained physician who specializes in treating cancer with radiation therapy.

Or technologist if there is any possibility that they are pregnant or if they are breastfeeding their baby.
Regarding pregnancy, breastfeeding, and imaging.
Patients with pacemakers or loose metal in their bodies should inform the treatment team if MRI is used for simulation or IGRT.
Reference markers or electromagnetic transponders may be placed inside the body, near or within the tumor, to help the treatment team identify the area.
Or tattooed with colored ink to help align and direct the radiation equipment.
Using ultrasound should drink enough water about an hour before each treatment to keep the bladder full so that the prostate can be imaged or “seen” by the ultrasound machine.
Aside from the routine preparation for radiation therapy, which may include three-dimensional conformal radiation therapy, intensity-modulated radiation therapy, proton beam therapy, or stereotactic body radiation therapy (SBRT).
The Proton Beam Therapy page, or the SBRT page for more information.
Generally, procedures are performed on an outpatient basis. However, it is advisable to prepare for spending half a day or more in the imaging department. You will be informed whether you will need someone to accompany you and take you home after the procedure.
You may be notified not to eat or drink anything after midnight before the treatment. Ask your doctor if you should continue taking your usual medications on the day of treatment and if you should bring your medications with you to the procedure.
How is the procedure performed?
Radiation surgery treatments are similar to taking X-rays. Generally, X-rays cannot be seen, felt, or heard, except for patients receiving treatment in the brain, who may see lights while the machine is on, even with their eyes closed. The treatment itself does not cause any pain or discomfort. If you experience pain for other reasons, such as back pain or discomfort from the head device or immobilization device, please inform the medical or nursing staff.

We are focused on the care of cancer patients, as a high-tech option to combat cancer. It also offers the best treatments through state-of-the-art equipment, combined with excellent human resources trained in the best Centers in the United States and Europe. With first-class equipment, we position ourselves as a reference center in the region, offering the best treatment without the need to travel outside the country.
Typically replies within a day
Hello, Welcome to the Affordable Cancer Care Costa Rica.( 9am-6 pm Cetral T.)