Stereotactic Radiosurgery (SRS) is a highly precise form of radiation therapy, initially developed to treat small tumors and functional abnormalities of the brain. Despite its name and compared to traditional radiation therapy, SRS is a non-surgical procedure that delivers highly focused radiation, at much higher doses, and in only one or a few treatments. This treatment is possible thanks to the development of highly advanced technologies that allow the delivery of maximum doses of radiation within the target, while minimizing the dose received by the surrounding healthy tissue, destroying the tumor and achieving maximum local control. SRS is used to treat many types of brain pathologies including: Benign or malignant tumors; primary and metastatic, whether single or multiple. Additionally, residual tumors after surgery; intracranial, orbital and skull base tumors; as well as arteriovenous malformations (AVM) and other conditions such as trigeminal neuralgia, etc.
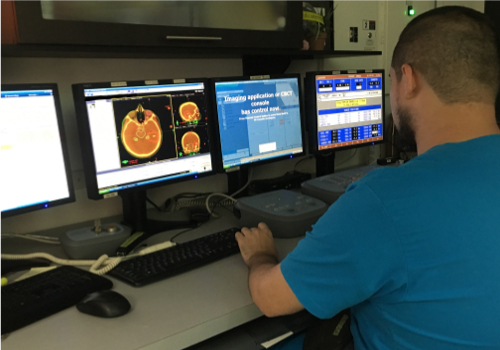

The treatment team is made up of several specialized medical professionals, typically radiation oncologists, a medical physicist, imaging scientists, a dosimetrist, and a radiation therapy nurse.
They are generally performed on an outpatient basis. However, it’s best to prepare to spend anywhere from half a day or more in the imaging department. You will be informed if you will need to have someone accompany you and drive you home after the procedure.
You may be told not to eat or drink anything after midnight before treatment. Ask your doctor if you should continue taking your regular medications on the day of treatment and if you should bring your medications with you to the procedure.
You are taking oral medications or use insulin to control diabetes.
You have an allergy to intravenous contrast media or iodine.
You have a pacemaker, artificial heart valve, defibrillator, brain aneurysm clamps, implantable chemotherapy pumps or ports, neurostimulators, eye or ear implants, stents, coils or filters.
Suffers from claustrophobia
1- When removing the device from the head there may be slight bleeding in the places where the screws were placed and they will be covered with a dressing. If you have a headache, you can ask for medicine to help you feel more comfortable.
2- In most cases, patients who have undergone radiosurgery and SRS can resume normal activities within one or two days.
3- Side effects of radiation therapy include problems that occur as a result of the treatment itself as well as damage done by the treatment to healthy cells in the treatment area.
4- The number and severity of side effects you experience depend on the type of radiation and dosage you receive and the part of the body undergoing treatment. You should talk to your doctor and nurse about any side effects you experience so they can help you manage them.
5- Radiotherapy can cause early side effects during or immediately after treatment, and they usually disappear within a few weeks. Late side effects may occur months or years later. Common early side effects of radiation therapy include tiredness or fatigue and skin problems. The skin in the treatment area may become more sensitive, red, irritated or swollen. Other skin changes include dryness, itching, peeling, and blistering.
There is a small risk of developing cancer from radiation therapy. After radiation therapy for cancer, you should undergo regular examination by your radiation oncologist to detect recurring and new cancers.
When using techniques such as SRS the goal is to maximize the cancer-destroying abilities of radiotherapy, while minimizing its effects on healthy tissues and organs, thereby avoiding the side effects of the treatment itself.
Donec feugat egestas quam in sollici tudine. Mauris and maxi mius dig nissim mauris, vel varus arcu auct or andy Praesent.
Donec feugat egestas quam in sollici tudine. Mauris and maxi mius dig nissim mauris, vel varus arcu auct or andy Praesent.
Donec feugat egestas quam in sollici tudine. Mauris and maxi mius dig nissim mauris, vel varus arcu auct or andy Praesent.
Donec feugat egestas quam in sollici tudine. Mauris and maxi mius dig nissim mauris, vel varus arcu auct or andy Praesent.
Donec feugat egestas quam in sollici tudine. Mauris and maxi mius dig nissim mauris, vel varus arcu auct or andy Praesent.
Suspendisse interdumnnec effiitur auctor, odio lcongue ligulaodales tortor turpis at elit. Aliquam iacipsum uttu odio variusid interdu lacae dictum. Mauris a maximus dolovestibulum.
Street 238,52 tempor
Donec ultricies mattis null
cipit risus tristique ut.
+1 500 000 0000
http://demo.com